What’s the news: The cut in physicians’ 2024 Medicare pay rates linked to Medicare’s budget-neutrality provision was three times more than it should have been, according to an AMA analysis of 2024 claims data.
The AMA is urging the Trump administration to correct a flaw in the formula used by the Centers for Medicare & Medicaid Services (CMS) that led to the pay cut before it results in a perpetual $1 billion shortfall to the annual Medicare physician payment schedule and a permanent across-the-board reduction to Medicare payment.
The flaw is a CMS overestimate for the use of its add-on complexity code for evaluation and management (E/M) services delivered in outpatient and office settings.
Unless an adjustment is made, this overestimate “will continue to threaten the sustainability of physician practices and access to care for America’s seniors and individuals with disabilities,” James L. Madara, MD, the AMA’s executive vice president and CEO, wrote in a letter (PDF) to Chris Klomp, the deputy administrator and director for CMS.
The AMA is leading the charge to reform the Medicare payment system.
Why it’s important: If CMS projects net cost changes for health services that boost Medicare spending by more than $20 million, the agency must reduce spending elsewhere in the annual Medicare physician payment schedule. This may be done by a downward adjustment to the Medicare conversion factor.
The AMA analysis shows that use of the CMS Healthcare Common Procedure Coding System (HCPCS) code G2211 was vastly overestimated. The code was projected to be billed with 38% of all outpatient and office E/M visits reported in 2024.
The AMA analysis, however, shows that G2211 was only reported in 10.5% of these visits during the first three quarters of 2024. Translated into a dollar figure, 2024 charges were around $390 million compared with the CMS projection of $1.3 billion — an overestimate that “is not without consequence,” Dr. Madara’s letter says.
“Because G2211 was implemented in a budget-neutral manner and was expected to increase Medicare spending drastically, it resulted in a steep, unwarranted cut to the Medicare conversion factor,” he wrote.
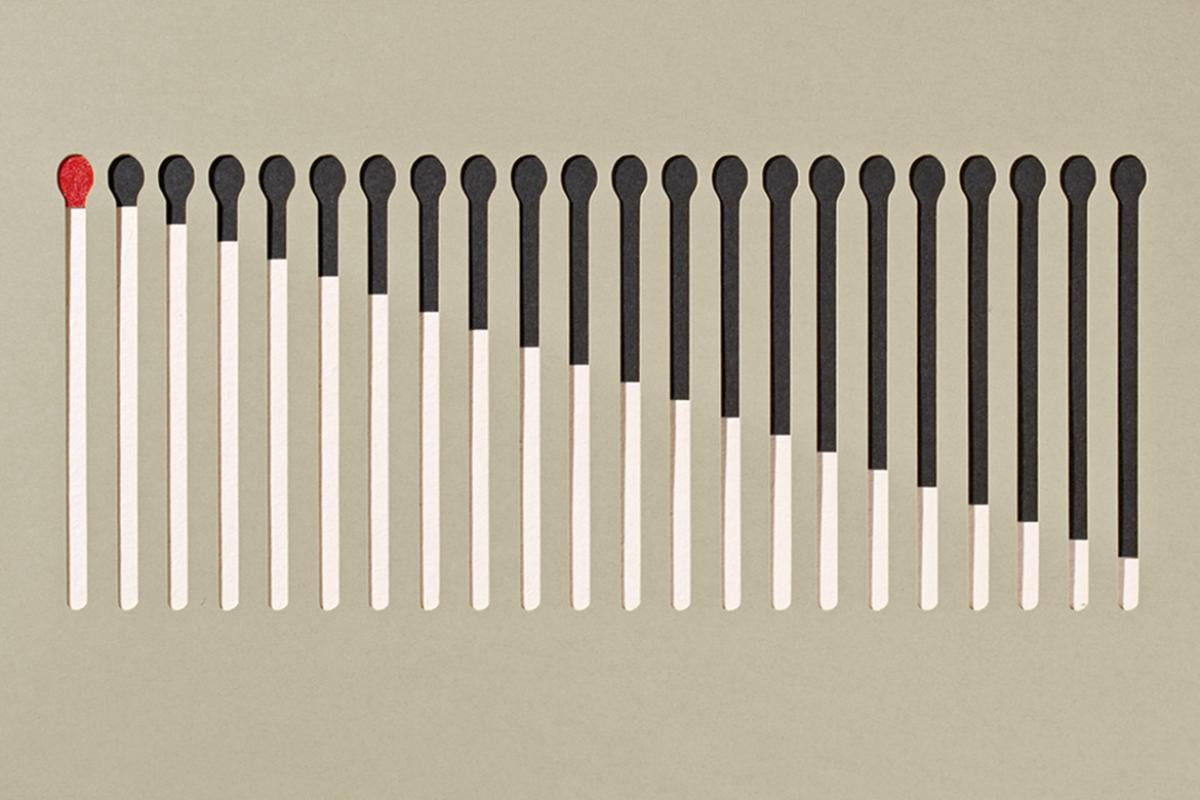
“Specifically, the budget-neutrality adjustment in the 2024 final rule resulted in a 2.18% decline to the 2024 conversion factor, but the actual 2024 claims data suggest this should have been 0.79%,” the AMA’s letter explains. “Therefore, the 2024 budget-neutrality adjustment cut was nearly three times as large as it should have been.”
This unwarranted budget neutrality cut coincides with an inflation-adjusted decline of 33% to Medicare physician payment since 2001.
Medicare’s trustees and the Medicare Payment Advisory Commission (MedPAC) have issued warnings about beneficiaries losing access to high-quality care due to insufficient Medicare physician payment.
“The AMA strongly urges CMS to correct the utilization estimate for G2211 based on actual claims data from 2024 by making a prospective budget neutrality adjustment to the 2026 conversion factor in the forthcoming 2026 Medicare physician payment schedule proposed rule,” Dr. Madara wrote.
Learn more: The AMA’s Fix Medicare Now campaign has generated more than half a million messages to Congress from patients and doctors.
Dive deeper to learn how Medicare pay cuts:
- Endanger physician practices.
- Threaten patients’ access to care.
- Especially affect rural America.
- Put even big medical groups at risk.
- Hit solo physician practices hard.
Explore the Medicare Basics series, which provides an in-depth look at important aspects of the Medicare physician payment system.